Temporomandibular joint diseases – sounds like a bunch of big words.
We demystified it for you below but first, here’s Mrs Haruna’s story…
Temporomandibular joint diseases
Mrs Haruna’s story
Mrs Haruna sat in her living room, on her antique couch. She ran her left hand over the Batik and felt the pattern with the tips of her fingers, stopped and ran her right hand on the couch instead.
She continued that way for a while until she caught herself doing it again, habitually. She placed her hands on the sides of her jaw and tried to still the movement. She continued to stare into space and clutched the Batik fabric instead, at least, that was better than clenching her teeth. The teeth-clenching tired her out, made the muscles of her face ache which only added more stress.

In her mind, she replayed some past events of her life; she had lost her husband less than a year ago, leaving behind one 24 yearold daughter who was studying in the United Kingdom. It was hard living all by herself at her home in Ikeja, Lagos, Nigeria. She did not have many friends or family members close by to spend time with. It was telling on her. Moments spent over video calls with her daughter became priceless but she couldn’t stay on the phone 24 hours a day. Her daughter, Zainab had her own life to live.
She discovered that she developed the habit of clenching her teeth over the past year, in trying to cope with sheer stress and she now ached on the sides of her face, in front of her ears. The pain came when she tried to chew, open or close her mouth.
She had been staring for 20 minutes when her phone rang,
Nene– “Hello” The high-pitched voice at the other end said.
She recognised the voice and shut her eyes in relief,
Mrs Haruna– “Nene, how are you?”
Nene was a sweet younger lady who had just moved a few houses away, they had met in a supermarket weeks before and became friends when they found out that they lived on the same street.
Nene– “Mrs Haruna, good evening Ma’am. I am fine. How are you doing today?”
Mrs Haruna– “Nene, you never get tired of doing this” Nene called every other day to find out about her wellbeing.
Nene– “It’s my pleasure Ma. How are you?”
Mrs Haruna– “I’ve got this pain in my jaw joint, it hurts when I try to open my mouth”
Nene– “Oh my, I am so sorry about that. Have you done anything about it?”
Mrs Haruna– “What do I do? I am not sure what to do.”
Nene– “Well, I’d say, you should see a dentist”
There was a Pause
Mrs Haruna– “Dentist? Never thought of that!”
Nene– “Yes ma, my father had that pain. They called it temporomandibular joint disease, something like that. But they helped him”
Mrs Haruna– “Okay Nene, any contacts?”
They did visit Schubbs Dental Clinics that week and it was a breeze. At the clinic, Mrs Haruna met the dentist who listened to her, examined her, and administered the therapy she needed.
Many people around the world suffer from temporomandibular joint diseases, most common among people between the ages 20 and 40, females are affected more than males. People who get the temporomandibular joint diseases experience pain and this pain is the second most common cause of pain in the face, after toothache.
These joint problems can be a source of concern and anxiety for people who suffer from it, but it’s nothing a visit to the dentist cannot help you with.
THE TEMPOROMANDIBULAR JOINT AND Temporomandibular joint diseases
In our bodies, joints are connections between bones that keep our skeleton in one piece. In general, joints found in the body allow you to walk, run, dance, play football and in one word, move.
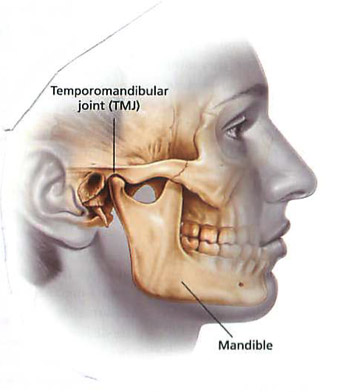
The temporomandibular joint is a hinge joint that connects your lower jaw to some bones in the sides of your skull, just in front of your ears. This joint allows you speak, sing, chew and yawn, in other words, it is the joint that lets you open your mouth and close it.
The temporomandibular joint is lined by some rubbery, flexible tissue (called cartilage), the joint also contains a lot of fluid, which allows some complex movements of the lower jaw. It is similar to some other joints in the body, having a covering around it called a capsule, an articular disc and some short bands of tough flexible tissue (ligaments) that help to keep the joint in place.
The articular disc is a thin, oval piece of tissue that separates the bones that make up the temporomandibular joint. This separation creates room in the joint space, allowing for movement and easing friction.
There are some very important muscles that are attached to and around the joint, the power and action of these muscles pull at the bones in the joint and cause movement.
The temporomandibular joint is such an important joint and any problem with it will affect anyone’s wellbeing and quality of life. Similar to the way a person can develop problems in his or her knee joint, elbow joint or vertebral joints in the spine, a person can have problems with the temporomandibular joint.
Temporomandibular diseases can be placed in two broad categories; true temporomandibular joint diseases and temporomandibular dysfunction syndrome.
The true temporomandibular joint diseases arise from the parts of the joint itself while the temporomandibular dysfunction syndrome can arise from the muscles around the joint, the nerves supplying the joint or even a psychological problem.
TEMPOROMANDIBULAR JOINT DISEASES
A problem with the temporomandibular joint may be as a result of a true temporomandibular joint disease or as a result of a temporomandibular dysfunction syndrome
Your dentist might diagnose you of a true temporomandibular joint disease if any of the following happen:
- A displacement of the articular disc
- Frequent dislocations of the joint, especially when it has happened over a long time
Dislocations occur when a joint is forced out of its normal position
- Forceful injury to the joint, these types of injuries may even break the bones that make up the joint
- Degenerative joint disorders such as Rheumatoid arthritis, septic arthritis, osteoarthritis and Lyme disease. An immune system disorder may also lead to this group of joint diseases.
- Fusion of the joint.
This results in an unusual stiffening of the joint that prevents movement of the joint
- Infections involving the joint
- A tumour arising from the joint
This can be caused by a variety of factors, most times it is a combination of factors.
- Stress and anxiety
- Habits
These habits include teeth grinding and jaw clenching habits. Sometimes, people clench their jaws to help them cope with stress. These habits put a lot of pressure on the joints.
- Personality disorders, for example, obsessive disorders
- Psychological problems from adverse life events
- Excessive yawning
- Poorly aligned teeth
- Poorly fitting dentures
- Poorly done dental restorations
- No known cause
Sometimes, the dentist may not be able to point out a particular cause.
The symptoms include:
- Pain on opening or closing your mouth
- Pain around your ears which may travel to the head, this pain is usually associated with chewing.
- A clicking or gritty sound from the joint
- Abnormal shifting of your lower jaw when you try to open or close your mouth
- Pain in the muscles around the joint
- An unusual movement of the muscle around the joint
- Complete or partial inability to open or close the mouth
- Severe headaches that do not go away even after taking pain medications
- Pain inside the ears
- Neck pain or stiffness
- Persistent problems with falling or staying asleep (insomnia)
The pain may be on one side of the face or on both sides, and may get severe during periods of stress.
TIPS FOR YOUR VISIT TO THE DENTAL CLINIC
If you have been experiencing what you think may be a temporomandibular joint disorder, it is about time you visited the dentist.
You will find below what you can expect, on your visit to the dental clinic.
The dentist will introduce himself or herself to you. He or she will also carry you along from start to finish.
He/she will take your history. You will be asked if you have experienced any of the described symptoms and if there has been a history of the above mentioned related conditions and causes.
He/she will carry out a physical examination, assessing your temporomandibular joint in the process.
He/she will examine your teeth, tongue and the rest of your mouth for anything abnormal or unhealthy. If your oral hygiene is not very good or if you have not done a routine scaling and polishing procedure to clean your teeth, you may have to do so.
Depending on what your dentist finds in the clinic, you may be asked to run some tests. The tests may include an x-ray, an ultrasound scan of the joint, a computed tomography scan, a magnetic resonance imaging or a special test called an arthroscopy.
If you have suffered from arthritis or any other joint disease in the past, you may be asked to run some blood tests to find out if the joint disease is also affecting your temporomandibular joint.
Most of the time, temporomandibular joint disorders will last for only a period and will not get worse.
Your dentist will counsel you and reassure you. He or she may prescribe pain medications or some muscle-relaxing medications.
If you have some dental restorations that are too high, your dentist may try to restore the balance. If you have a tooth clenching habit, your dentist may prescribe a mouth guard especially for use at night. If your teeth are not well aligned, you may need braces. Your dentist will also likely recommend some physiotherapy for you.
In extreme cases, surgery is required.
The dentist may make the following recommendations for home care:
- Eat a soft diet and cut your foods into small bite sizes.
- Avoid chewing foods like chewing gum, bone, ice or raw carrots.
- Use moist heat or cold packs. Ask your dentist how.
- Avoid excessive or extreme jaw movements
- Keep your teeth apart as much as you can to prevent pressure on the jaw
- You can do some mild jaw exercises or massages if your dentist and physiotherapist think it is okay to do it
- Practice relaxation training. Your physiotherapist will show you how.
FAQ
That’s possible since the joint is still in use. Pay a visit to the dentist once this happens, don’t try to treat yourself.
In this season of the COVID-19 pandemic, stress may be creeping up your neck and it now seems easy to ignore your oral health.
Stress can lead to a number of oral health problems as well as other health issues, one more reason to get checked.
Good oral health improves anyone’s quality of life, one step in the right direction is a visit to the dentist.
Book an appointment with one of our dentists today!

